Guided Tissue Regeneration (GTR) is a dental procedure promoting the repair of damaged tissues, utilizing barrier membranes to direct healing. Key CDT codes include D4266 and D4267.
1.1 Definition and Purpose of GTR in Dentistry
Guided Tissue Regeneration (GTR) is a dental procedure that promotes the repair of damaged periodontal and bone tissues. It involves using barrier membranes to direct healing, preventing epithelial and connective tissue invasion into defect areas. The primary purpose of GTR is to regenerate lost bone and attachment structures around teeth or implants, enhancing functional and esthetic outcomes. This technique is critical for treating periodontal defects and ensuring optimal healing, often utilizing CDT codes like D4266 and D4267 for precise billing and documentation.
1.2 Historical Background and Evolution of GTR
Guided Tissue Regeneration (GTR) emerged as a revolutionary approach in dentistry during the late 20th century, evolving from periodontal regeneration research. Initial concepts involved non-resorbable barriers, which required secondary procedures for removal. Advances in biomaterials led to the development of resorbable membranes, simplifying the process. The introduction of CDT codes like D4266 and D4267 standardized billing for these procedures. Over time, GTR has become a cornerstone in treating periodontal defects and enhancing bone regeneration, with ongoing research refining techniques and materials for improved outcomes.

Dental Codes Related to Guided Tissue Regeneration
Dental codes D4266 and D4267 are used for guided tissue regeneration with resorbable and non-resorbable barriers, respectively, aiding in accurate billing and insurance claims.
2.1 CDT Code D4266: Guided Tissue Regeneration ⏤ Resorbable Barrier
CDT Code D4266 applies to guided tissue regeneration procedures using a resorbable barrier. This code is used when a biocompatible, absorbable membrane is placed to promote healing and tissue repair. The procedure involves positioning the membrane to guide the growth of new tissue, such as bone or periodontal ligament, in areas damaged by disease or trauma. Importantly, this code does not include flap entry, closure, or wound debridement, distinguishing it from other GTR-related codes.
2.2 CDT Code D4267: Guided Tissue Regeneration ⏤ Non-Resorbable Barrier
CDT Code D4267 is assigned to guided tissue regeneration procedures utilizing a non-resorbable barrier. This code applies when a durable, non-absorbable membrane is placed to facilitate tissue repair, typically in periodontal defects or around dental implants. Unlike resorbable barriers, non-resorbable membranes require removal in a separate procedure, which is included in this code. D4267 is used per site and is essential for cases where long-term tissue guidance is necessary to achieve optimal healing outcomes.
2.3 Other Relevant Codes and Their Applications
Beyond D4266 and D4267, other codes like D7953 (bone graft for ridge preservation) and D6106/D6107 (guided tissue regeneration for implants) are relevant. D4265 may also apply for supportive GTR services. These codes ensure accurate billing for various GTR procedures, including bone grafts and implant-related tissue regeneration. Proper code selection is crucial for reimbursement and documentation accuracy in dental practices.

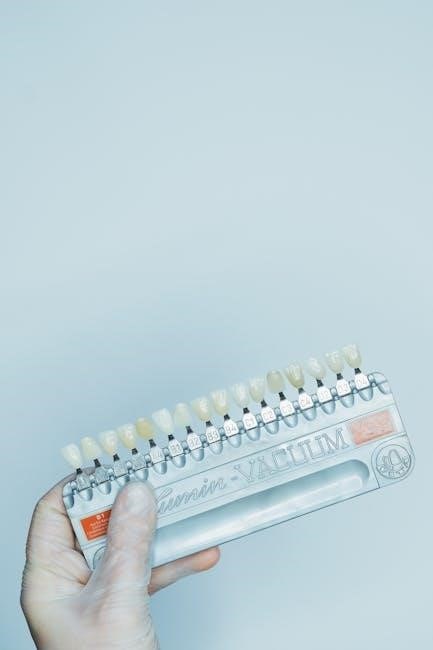
Materials and Membranes Used in GTR
GTR employs resorbable and non-resorbable membranes, such as collagen or titanium, to guide tissue healing. These materials are selected based on their biocompatibility and degradation properties.
3.1 Resorbable vs. Non-Resorbable Membranes
Resorbable membranes, like collagen or synthetic polymers, degrade naturally, eliminating the need for removal. They promote healing without secondary surgery, reducing patient discomfort. Non-resorbable membranes, such as titanium or PTFE, are durable and provide long-term support but require removal, increasing the risk of complications. The choice between them depends on the clinical scenario, defect size, and patient-specific factors. Resorbable membranes are preferred for their bioactivity and integration with surrounding tissue, while non-resorbable options offer structural stability for complex cases.
3.2 Characteristics and Selection Criteria for Membranes
Membrane selection in GTR depends on material, biocompatibility, and degradation properties. Resorbable membranes, such as collagen, offer biocompatibility and eliminate removal needs, while non-resorbable options like titanium provide durability. Factors like defect size, healing goals, and patient health guide choices. Membranes must ensure space maintenance, tissue integration, and minimal immune response. Clinicians assess these characteristics to optimize outcomes, balancing material properties with clinical requirements for successful tissue regeneration and patient comfort, ensuring tailored treatment approaches for each case, enhancing predictability and success rates significantly in dental procedures. Proper selection is crucial for optimal healing and minimizing complications, ensuring the best possible results tailored to individual patient needs and specific dental conditions, thus playing a pivotal role in the effectiveness of guided tissue regeneration therapies.
Clinical Applications of Guided Tissue Regeneration
Guided tissue regeneration is used for periodontal regeneration, peri-implant tissue repair, and ridge augmentation, addressing defects and restoring dental function and aesthetics effectively.
4.1 Periodontal Tissue Regeneration
Guided tissue regeneration (GTR) is widely used in periodontal therapy to restore damaged tissues around natural teeth. By placing barrier membranes, GTR promotes the growth of new periodontal ligament and bone. Resorbable and non-resorbable membranes guide healing, preventing epithelial invasion. This technique is particularly effective in treating periodontal defects, enhancing attachment levels, and improving oral function. Procedures are coded using CDT codes like D4266 (resorbable barrier) and D4267 (non-resorbable barrier), ensuring accurate billing and documentation.
4.2 Peri-Implant Tissue Regeneration
Guided tissue regeneration (GTR) plays a crucial role in peri-implant tissue regeneration, addressing defects around dental implants. By using resorbable or non-resorbable membranes, GTR prevents soft tissue infiltration, promoting bone and ligament growth. This technique is particularly effective in managing peri-implantitis and enhancing implant stability. Procedures are coded using CDT codes D4266 (resorbable barrier) and D4267 (non-resorbable barrier), ensuring precise documentation and billing for implant-related tissue regeneration treatments.
4.3 Ridge Augmentation and Bone Regeneration
Guided tissue regeneration (GTR) is instrumental in ridge augmentation, addressing insufficient bone volume for dental implants. Using resorbable barriers, GTR directs bone growth, enhancing the alveolar ridge’s width and height. This method is particularly effective in cases of severe bone resorption. The procedure involves placing a membrane to prevent soft tissue ingrowth, allowing bone cells to regenerate. Coded under D4266 for resorbable barriers, GTR ensures predictable bone regeneration, facilitating successful implant placement and restoring aesthetic and functional outcomes.

Procedure and Technique in GTR
Guided Tissue Regeneration involves surgical steps, placement of resorbable or non-resorbable membranes, and stabilization techniques to ensure proper bone or tissue healing effectively.
5.1 Surgical Steps and Protocol
The procedure begins with patient preparation and local anesthesia. A mucosal incision is made to access the defect site, followed by thorough debridement of diseased tissue. A resorbable or non-resorbable membrane is placed over the defect, stabilized using sutures or bone tacks. The flap is closed to secure the membrane, and wound debridement may be performed if indicated. Proper membrane stabilization is critical for preventing displacement and ensuring effective tissue regeneration. This step is coded under D4266 or D4267, depending on the membrane type.
5.2 Membrane Placement and Stabilization
Membrane placement is critical for GTR success. The barrier is positioned over the defect, ensuring complete coverage and proper adaptation. Stabilization is achieved using sutures, bone tacks, or titanium pins to prevent displacement. The membrane must be tightly secured to maintain space for tissue growth. Resorbable membranes integrate naturally, while non-resorbable ones require removal later. Proper fit and stabilization minimize complications, such as membrane exposure or failure, ensuring optimal healing outcomes. This step is essential for directing tissue regeneration effectively.
5.3 Follow-Up and Membrane Removal
Post-operative follow-up is crucial for monitoring healing progress. Non-resorbable membranes typically require removal 4–6 weeks after placement, under local anesthesia. The procedure involves careful extraction to avoid tissue damage. Resorbable membranes eliminate the need for removal, reducing patient discomfort and procedure costs. Regular check-ups ensure proper healing and prevent complications. Proper documentation, including CDT codes like D4266 and D4267, is essential for accurate billing and insurance reimbursement, ensuring streamlined administrative processes for dental practices.
Success Rates and Predictable Outcomes
Guided Tissue Regeneration (GTR) demonstrates high success rates, with predictable outcomes in bone and soft tissue regeneration. Proper technique and membrane selection enhance healing efficiency and patient satisfaction.
6.1 Factors Influencing the Success of GTR
Success in Guided Tissue Regeneration is influenced by patient-specific factors such as oral hygiene, bone quality, and compliance. Membrane choice, surgical technique, and follow-up care are critical. Resorbable barriers (CDT D4266) and non-resorbable barriers (CDT D4267) have different outcomes based on tissue type. Proper coding ensures accurate documentation and insurance coverage, while patient education enhances healing. Early intervention and tailored treatment plans improve predictability and long-term tissue regeneration success rates.
6.2 Clinical Evidence and Case Studies
Clinical studies demonstrate high success rates for GTR procedures, with resorbable barriers (CDT D4266) showing comparable outcomes to non-resorbable barriers (CDT D4267). Case studies highlight effective bone and tissue regeneration in periodontal defects and implant sites. Patient-specific factors, such as compliance and bone quality, significantly impact results. Research supports the use of GTR for achieving predictable outcomes, with minimal complications when proper techniques are applied. Documented success includes rapid healing, minimal scarring, and optimal tissue regeneration, making GTR a reliable treatment option in modern dentistry.

Coding Guidelines and Insurance Considerations
Proper coding ensures accurate reimbursement. Use CDT codes D4266 and D4267 based on membrane type. Verify insurance coverage and obtain pre-authorization for GTR procedures.
7.1 Proper Coding Practices for GTR Procedures
Accurate coding is essential for GTR procedures. Use CDT codes D4266 for resorbable barriers and D4267 for non-resorbable barriers. Ensure codes reflect the membrane type and site specifics. Document whether the procedure involves natural teeth or implants. Note that D4266 excludes flap entry and closure, while D4267 includes membrane removal. Always verify patient-specific details and procedure complexity for correct code selection and reimbursement.
7.2 Insurance Reimbursement and Billing Tips
For GTR procedures, ensure accurate billing by submitting CDT codes D4266 or D4267, reflecting the membrane type used. Verify insurance coverage pre-procedure, as policies vary. Document clinical necessity and attach supporting diagnostics. Submit detailed reports, including pre- and post-op images, to justify the procedure. Itemize bills clearly, separating GTR from other services. Patient education on costs and insurance benefits is crucial for transparency. Follow-up with insurers to address any claims issues promptly.

Complications and Risks Associated with GTR
Common complications include membrane exposure, infection, and incomplete tissue regeneration. Patient-specific risks such as poor healing or systemic conditions may affect outcomes. Proper technique minimizes these issues.
8.1 Common Complications and Their Management
Complications in GTR include membrane exposure, infection, and incomplete regeneration. Exposure often leads to contamination and failure. Management involves debridement and antibiotic therapy. Infection control is crucial for success. Proper surgical technique and patient compliance reduce risks. Early detection and intervention are key to managing these complications effectively, ensuring optimal healing outcomes for patients undergoing GTR procedures.
8.2 Patient-Specific Risk Factors
Patient-specific risk factors for GTR include smoking, poor oral hygiene, and systemic conditions like diabetes, which impair healing. Severe periodontal disease and low bone density also increase failure risks. Non-compliance with post-operative instructions can hinder regeneration. Individual anatomical challenges, such as insufficient keratinized tissue, may affect outcomes. Accurate patient selection and personalized treatment planning are critical to minimize these risks and enhance the success of guided tissue regeneration procedures.

Advancements and Future Directions in GTR
Emerging technologies include bioabsorbable membranes, growth factors, and 3D printing, enhancing predictability and customization in GTR. Research focuses on stem cell therapies and advanced biomaterials for improved outcomes.
9.1 Emerging Technologies and Materials
Emerging technologies in GTR include bioabsorbable membranes, growth factors, and 3D-printed scaffolds, enhancing tissue repair. Advanced materials like nanofiber membranes and stem cell therapies are being explored. These innovations aim to improve predictability and customization, reducing healing times. Additionally, researchers are developing smart membranes that release bioactive molecules, promoting faster regeneration. Standardization efforts, such as ISO 22803, ensure material safety and efficacy, paving the way for next-generation GTR treatments.
9.2 Research and Development in GTR
Research in GTR focuses on improving predictability and outcomes, with studies on bioactive molecules, tissue engineering, and advanced membrane materials. Systematic reviews and clinical trials evaluate the efficacy of resorbable vs. non-resorbable barriers. Recent studies highlight the role of vitamin D in enhancing bone regeneration and osseointegration. Additionally, ISO 22803 standards guide the development of membrane materials for oral surgery. These advancements aim to optimize tissue repair and provide evidence-based solutions for complex dental cases, ensuring safer and more effective treatments.

Patient Education and Post-Operative Care
Patient education is crucial for optimal healing. Emphasize compliance with post-operative instructions to ensure proper tissue regeneration and minimize complications, fostering successful GTR outcomes.
10.1 Patient Instructions for Optimal Healing
Patients should follow specific post-operative instructions to ensure proper healing after GTR. These include a soft food diet for several weeks, avoiding direct brushing near the surgical site, and rinsing with saline or antibacterial mouthwash. Smoking and heavy physical activity should be avoided to prevent complications. Patients are advised to attend all scheduled follow-up appointments and adhere to prescribed medications for pain management. Compliance with these instructions is critical for achieving predictable outcomes and minimizing the risk of membrane exposure or failure.
10.2 Importance of Compliance in GTR Outcomes
Compliance with post-operative instructions is crucial for successful GTR outcomes. Non-compliance can lead to complications such as membrane exposure or infection, potentially compromising healing. Adhering to dietary restrictions, hygiene practices, and follow-up appointments ensures optimal tissue regeneration. Patient cooperation in avoiding harmful habits, like smoking, further enhances healing. Proper compliance maximizes the effectiveness of GTR, leading to predictable and favorable clinical results. It is essential for patients to understand their role in achieving successful tissue regeneration and long-term oral health.
